Ever wished you could expand your dental practice’s offerings and make a real difference in people’s lives? Look no further than DSM Solutions for dental sleep medicine training.
This rapidly growing field allows you to treat sleep disorders like sleep apnea, a condition affecting millions and often undiagnosed. By incorporating dental sleep medicine into your practice you’ll not only attract new patients, but also improve the health and well-being of your existing ones.
New Patients with a Unique Service
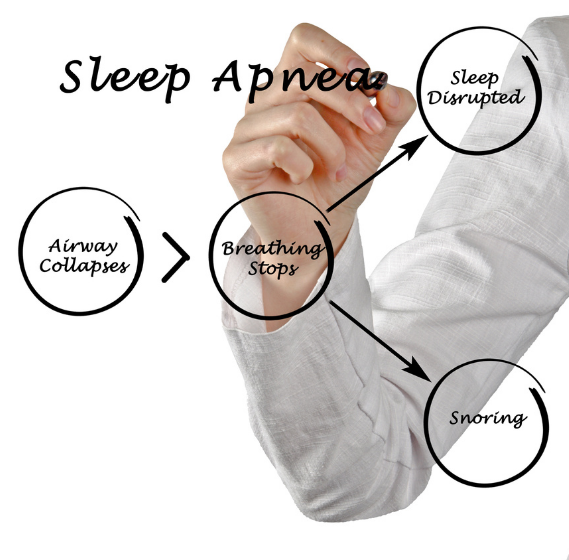
In today’s competitive dental landscape, standing out from the crowd is crucial. Dental sleep medicine offers a unique service that can set you apart. Many people suffer from sleep apnea, often undiagnosed, and struggle with CPAP machines – the traditional treatment. You can provide a comfortable alternative with custom-made oral appliances that gently hold the airway open during sleep.
DSM Solutions for Your Practice
The path to offering dental sleep medicine starts with education. DSM Solutions offers training courses for the entire team, not just the doctor.
The training will equip you with the skills to identify and screen patients for sleep apnea, understand the anatomy of the airway, and fabricate or fit oral appliances. Many programs also cover billing and insurance coding specific to dental sleep medicine.
How Dental Sleep Medicine Helps Your Patients
By incorporating dental sleep medicine, you’ll be offering your patients a life-changing service. Sleep apnea disrupts sleep, leading to daytime fatigue, mood swings, and even health complications like heart disease. Treating sleep apnea with an oral appliance can dramatically improve patients’ quality of life.
Here’s a glimpse of the benefits you’ll be providing:
- Improved Sleep:Oral appliances keep the airway open, allowing for better sleep quality. Patients report feeling more rested and energized throughout the day.
- Reduced Daytime Fatigue:With proper sleep, patients experience less daytime sleepiness, leading to increased focus and productivity.
- Enhanced Mood:Sleep apnea can contribute to irritability and depression. Treatment can lead to a more positive outlook and improved emotional well-being.
- Healthier Lifestyle:Treating sleep apnea can lower the risk of heart disease, stroke, and other health problems associated with chronic sleep deprivation.
The Next Step: Embracing Dental Sleep Medicine
Working with DSM Solutions presents a win-win situation. You’ll expand your practice’s capabilities, attract new patients seeking this valuable service, and most importantly, contribute to your patients’ overall health and well-being.
By investing in DSM Solutions training and incorporating this service, you’ll be taking a significant step towards becoming a leader in comprehensive patient care.